
Sciatica vs piriformis syndrome is a comparison many people search for when pain begins in the lower back or buttock and travels down the leg. The symptoms can feel similar, yet the underlying causes are different, which is why choosing the right approach to care matters.
Understanding the difference between these two conditions can help you avoid ineffective treatments, reduce frustration, and take steps that better support recovery. In this guide, we will explain how they differ, how clinicians tell them apart, and what treatment strategies are commonly recommended.
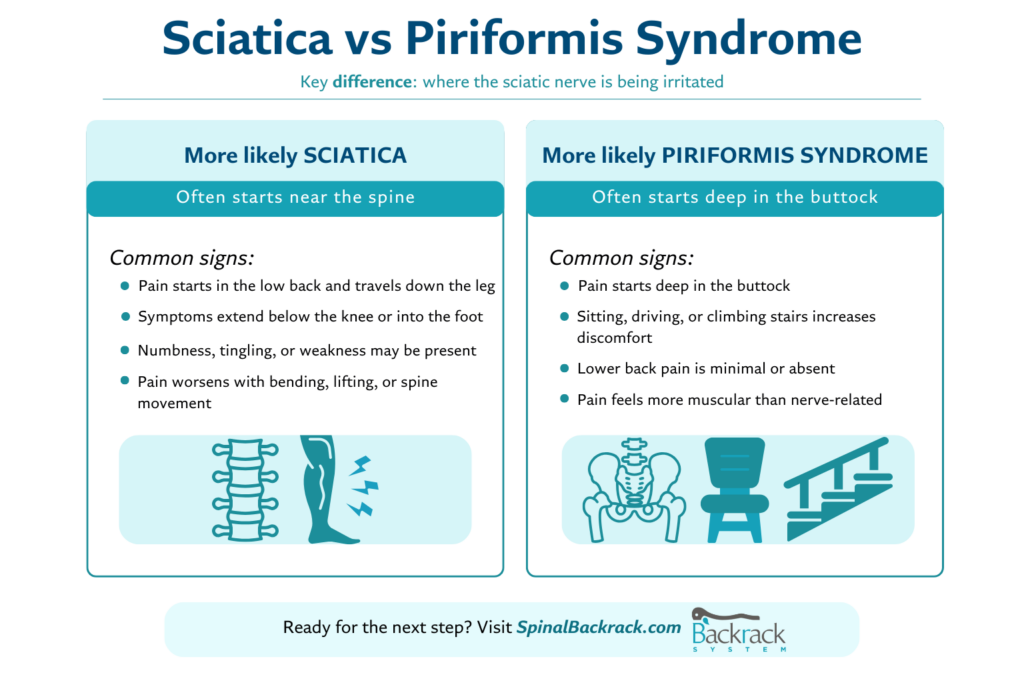
When comparing sciatica vs piriformis syndrome, the key difference is where the sciatic nerve becomes irritated.
You may be dealing with sciatica if:
You may be dealing with piriformis syndrome if:
Sciatica is not a diagnosis itself but a set of symptoms caused by irritation or compression of the sciatic nerve, most often near the spine.
When spinal nerve roots are compressed, pain may radiate from the lower back through the buttock and down the leg.
It’s piriformis syndrome when that deep buttock muscle presses on the sciatic nerve and triggers pain or tingling.
Unlike spinal sciatica, this condition originates in the hip and gluteal region rather than the spine.
The sciatic nerve runs from the lower spine, through the pelvis, and down the leg. Because it passes close to the piriformis muscle, irritation can occur either at the spine or in the deep gluteal region.
This overlap explains why sciatica vs piriformis syndrome is frequently misidentified without proper assessment.
Trigger patterns also differ. Spinal movement tends to worsen sciatica symptoms, while sitting and hip rotation more often aggravate piriformis-related pain.
These checks cannot diagnose sciatica vs piriformis syndrome, but they can help identify patterns worth discussing with a clinician.
Stop if symptoms worsen or neurological signs appear.
Healthcare providers rely on movement-based assessments to differentiate sciatica vs piriformis syndrome.
Pain reproduction during this test often points to spinal nerve root involvement.
This hip-based test may reproduce symptoms linked to piriformis-related sciatic nerve irritation.
Imaging may identify spinal causes but is often used to rule out other conditions rather than confirm piriformis syndrome.
Other issues can produce similar symptoms, including:
Persistent or worsening pain should always be evaluated.
Seek medical care promptly if you experience:
Treatment depends on whether symptoms stem from spinal compression or muscular irritation.
For spinal-related symptoms:
For piriformis-related symptoms:
All exercises should remain comfortable and controlled.
When spinal compression contributes to symptoms, gentle decompression may help reduce pressure on spinal structures.
Used appropriately, it can support symptom management for some people dealing with sciatica vs piriformis syndrome, alongside movement and strengthening.
Professional guidance is recommended when symptoms are severe or unclear.
Understanding sciatica vs piriformis syndrome can help guide which at-home tools may be appropriate. Spinal decompression devices like Backrack are designed to support gentle unloading of the spine as part of a balanced spine care routine.
These tools are intended to complement, not replace, professional care.
Yes. Irritation near the piriformis muscle can compress the sciatic nerve and reproduce symptoms similar to sciatica.
Not always. While the source is typically spinal, some people mainly notice leg symptoms.
Recovery varies, but symptoms often improve with consistent movement modification and strengthening.
Side sleeping with proper support or maintaining a neutral spinal position often reduces strain.
A clear understanding of sciatica vs piriformis syndrome allows you to move away from guesswork and toward more effective care decisions. By recognizing symptom patterns, understanding triggers, and combining professional guidance with responsible at-home strategies, you can better support long-term spinal and nerve health.








Sign up our newsletter to get article update about backrack therapy.