If you are asking who is spinal decompression best for, you are already doing the smartest thing you can do: pausing to make sure it fits your symptoms, your comfort level, and your safety. Spinal decompression can be a helpful part of an at-home routine for certain patterns of back and leg discomfort, but it is not for everyone, and it is not something you should force.
This guide will help you quickly figure out whether decompression is likely a good match for you, who should avoid it (or get checked first), what results to expect, and how to start gently and safely.
Important: This article is educational, not medical advice. If you have severe symptoms, symptoms that are getting worse, or any red flags listed below, get evaluated by a qualified healthcare professional.
If you’re still deciding who is spinal decompression best for, our spinal decompression device can support a gentle, repeatable at-home routine.
Spinal decompression is a gentle approach that aims to reduce pressure and tension through the lower back by “unloading” the spine. People often describe it as a feeling of lengthening, relief, or a mild stretch combined with relaxation.
If you want a quick overview of what it is and what it is not, see our spinal decompression therapy explained guide.
What it is:
What it is not:
There are many ways decompression can be done, including clinical traction, physical therapy techniques, and at-home decompression routines. The method matters, but so does the person. That is why the “who is it best for” question is so important.
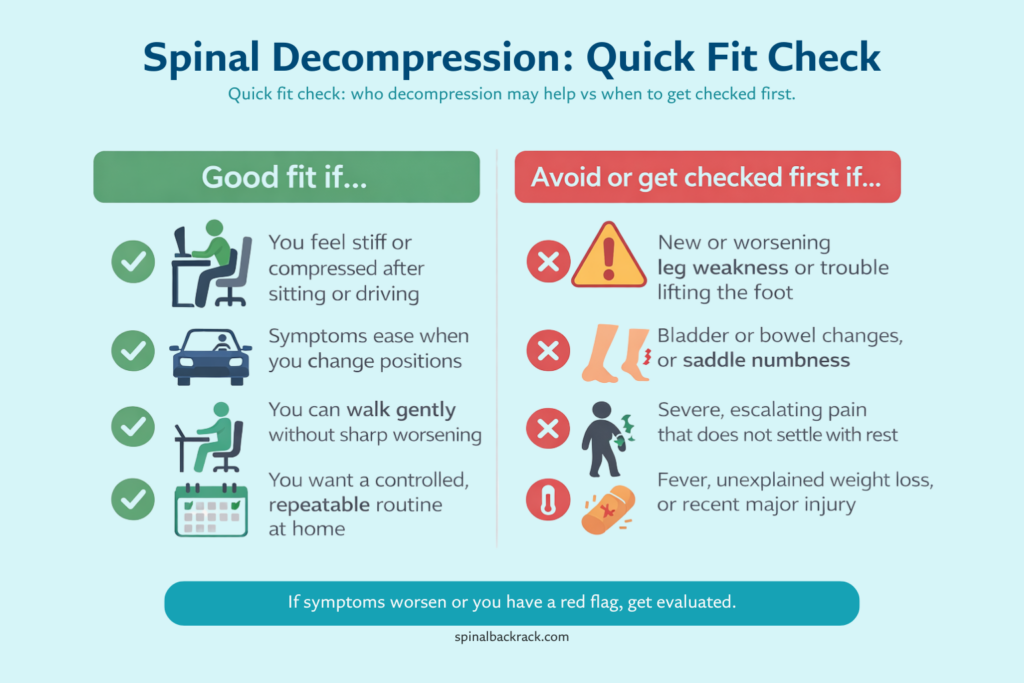
Below are the most common “good fit” patterns. You do not need to match all of them. If a few sound like you and you can do gentle unloading without worsening symptoms, decompression may be worth trying as part of a broader routine.
This is one of the most common groups.
You might relate if:
Why decompression may help:
Best approach:
This is a big clue that your symptoms are “position sensitive.”
You might relate if:
Why decompression may help:
Best approach:
Sciatica-like symptoms can include buttock pain, tingling, burning, or pain that travels down the leg. Decompression may help some people, especially if symptoms calm when pressure is reduced.
You might relate if:
Important caution: If decompression makes symptoms sharply worse or causes the pain to travel farther down the leg, stop and reassess.
Best approach:
Some people describe their pain as “disc-related,” often with sitting sensitivity and irritation from bending or lifting. Decompression can be helpful for some, but only when it is gentle and symptoms are stable.
You might relate if:
Best approach:
This matters more than most people think. A routine that is “pretty good” but done consistently often beats a routine that is “perfect” but rarely done.
You might relate if:
Best approach:
This section is here to protect you, and to help you make an informed decision.
Seek urgent evaluation if you have any of these:
These are red flags that need professional assessment.
Decompression may still be possible for some people, but you should not guess.
Talk to a clinician if you have:
When in doubt, it is better to get guidance than to push through.
Use this as a simple, practical guide. It is not a diagnosis.
If this is you, start with very short sessions and track your response.
If any of these happen, stop and consider medical evaluation.
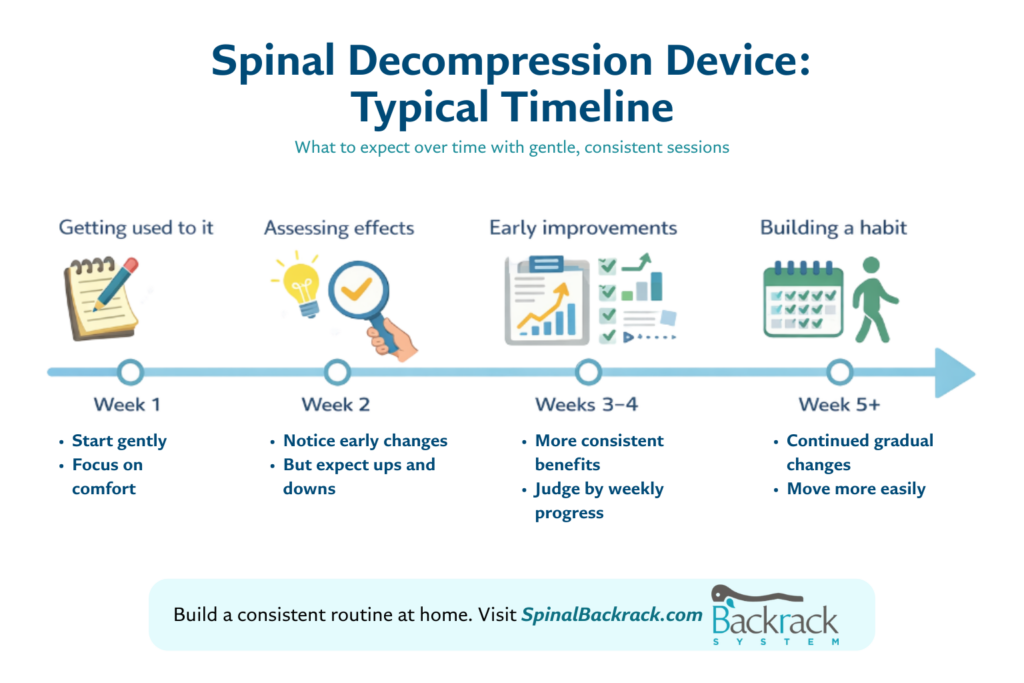
This is where many people get frustrated. They try one session, do not feel “fixed,” and give up. Decompression is usually not an instant cure. It is more like a habit that can gradually reduce stiffness, calm sensitivity, and improve tolerance over time.
A realistic timeline looks like this for many people:
Possible improvements:
Possible non-improvement: No big change, especially if you are very irritated that day
Possible improvements:
Possible improvements:
Possible improvements:
Why results vary:
This is the simple approach that fits most people.
Do not chase intensity. A mild session done consistently is often better than a “hard” session done rarely.
Discomfort is not the same as sharp, radiating pain. If symptoms intensify or spread, stop.
Decompression works best when combined with:
Day 1 to 3:
Day 4 to 7:
Week 2 and beyond:
An at-home decompression device can be helpful if you want a controlled, repeatable routine without needing appointments or complicated setups. The key is to use it as part of a calm plan, not as a “more is better” solution.
Most readers start with the Backrack device. The combo is optional if you want added lumbar support.


Tip: Start gently. Consistency matters more than intensity.
Our device tends to be a good fit for people who:
How it supports your routine:
Safety reminder: If you have red flags, severe symptoms, or significant medical risk factors, get evaluated before attempting decompression at home.
It is usually best for people who feel compressed or stiff from sitting, and who get at least some relief when they change positions or walk gently. It tends to work best when done gently and consistently, alongside simple movement habits.
Avoid decompression and get checked urgently if you have loss of bowel or bladder control, saddle numbness, new or worsening weakness, or severe unchanging pain. If you have major risk factors like severe osteoporosis, recent surgery, or worsening neurological symptoms, speak with a clinician first.
It can be safe for many people when it is gentle, controlled, and stopped if symptoms worsen. It is not safe to push through sharp radiating pain, increasing numbness, or new weakness.
Some people feel temporary relief after a session, but meaningful improvement usually takes consistent practice over weeks. Many people notice changes within 2 to 4 weeks, with more stable progress over 6 to 8 weeks when combined with movement habits.
Most people do best with short, gentle sessions performed consistently. Start with a few times per week or daily short sessions if tolerated, then adjust based on your response.
Yes, especially if you do too much too fast, or if your symptoms are highly irritable. If pain intensifies, travels farther down the leg, numbness increases, or weakness appears, stop and get evaluated.
If you want a straightforward plan this week:
If you are still deciding who is spinal decompression best for, use the checklists above, start gently, and choose an at-home routine you can actually stick with.
Further reading:





Sign up our newsletter to get article update about backrack therapy.